Page Contents
ToggleIntroduction:-
Mnemonic FAST HUGS BID serves as a comprehensive checklist for healthcare providers to ensure that all essential care components are addressed daily in critical care settings.
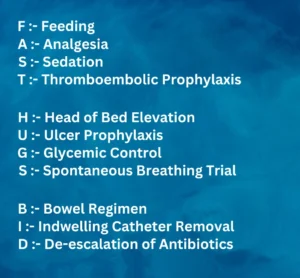
This detailed guide breaks down each aspect of FAST HUGS BID, providing thorough explanations of interventions and implications for patient care.
F: Feeding:-
Intervention:
-
Nutritional Assessment:-
Conduct a thorough assessment of the patient’s nutritional status upon admission and regularly throughout their stay. This includes evaluating weight, body mass index (BMI), serum albumin levels, and other relevant markers.
-
Determine Feeding Method:-
Decide the best method of feeding based on the patient’s condition. Options include oral feeding, enteral nutrition (tube feeding), or parenteral nutrition (intravenous feeding). Enteral nutrition is preferred when the gastrointestinal tract is functional because it supports gut integrity and immune function.
- Caloric Monitoring: Regularly monitor the patient’s caloric intake and adjust as necessary to meet their metabolic needs. This involves calculating the patient’s daily caloric requirements and ensuring they receive adequate protein, fats, carbohydrates, vitamins, and minerals.
Implication:-
- Proper nutrition is fundamental for recovery, particularly in critically ill patients who have increased metabolic demands. Malnutrition can delay healing, increase susceptibility to infections, and prolong hospitalization. Providing adequate nutrition supports immune function, preserves muscle mass, and enhances wound healing, thereby improving overall outcomes.
A: Analgesia:-
Intervention:-
- Pain Assessment: Regularly assess the patient’s pain using appropriate pain scales such as the Numeric Rating Scale (NRS) or the Critical-Care Pain Observation Tool (CPOT) for non-verbal patients.
- Pain Management Strategies: Administer analgesics based on the pain assessment. Options include opioids (e.g., morphine, fentanyl), non-opioid analgesics (e.g., acetaminophen, NSAIDs), and adjunctive therapies (e.g., gabapentin, ketamine). Non-pharmacological methods like relaxation techniques, music therapy, or cold/heat therapy can also be beneficial.
- Adjustments and Monitoring: Continuously monitor the effectiveness of pain management strategies and adjust dosages or medications as needed. Be vigilant for signs of over-sedation, respiratory depression, or other side effects.
Implication:-
- Effective pain management is crucial for patient comfort and can reduce stress, anxiety, and physiological responses that may negatively impact recovery. Uncontrolled pain can lead to increased heart rate, hypertension, and elevated stress hormone levels, which can impede healing and prolong ICU stays. Appropriate analgesia improves overall patient satisfaction and promotes faster recovery.
S: Sedation:-
Intervention:-
- Sedation Assessment: Use validated sedation scales such as the Richmond Agitation-Sedation Scale (RASS) to regularly assess the patient’s sedation level.
- Sedation Management: Administer sedative medications (e.g., propofol, dexmedetomidine, benzodiazepines) to achieve the desired level of sedation. Tailor the sedation plan to the patient’s needs, balancing adequate sedation with the risk of oversedation.
- Daily Sedation Vacations: Implement daily sedation vacations, where sedation is temporarily reduced or stopped to assess the patient’s neurological status and readiness for weaning off sedation.
Implication:-
- Proper sedation management is essential to ensure patient comfort, reduce anxiety and agitation, and facilitate necessary medical interventions. However, oversedation can lead to prolonged mechanical ventilation, increased risk of infections, and longer ICU stays. Regular assessment and sedation vacations help balance sedation needs and promote faster recovery and shorter ICU duration.
T: Thromboembolic Prophylaxis:-
Intervention:-
- Risk Assessment: Assess the patient’s risk for thromboembolic events using tools such as the Padua Prediction Score or Caprini Risk Assessment Model.
- Prophylactic Measures: Implement appropriate prophylactic measures based on the risk assessment. Pharmacological options include anticoagulants like heparin or enoxaparin. Mechanical prophylaxis includes compression stockings or pneumatic compression devices or DVT Pump also .
- Ongoing Evaluation: Regularly evaluate the effectiveness of prophylactic measures and adjust them as necessary. Monitor for signs of bleeding or adverse reactions to anticoagulants.
Implication:-
- Preventing thromboembolic events is critical in critically ill patients who are often immobile and at higher risk for deep vein thrombosis (DVT) and pulmonary embolism (PE). Effective prophylaxis reduces the incidence of these potentially life-threatening complications, thereby enhancing patient safety and improving outcomes.
H: Head of Bed Elevation:-
Intervention:-
- Positioning: Ensure the head of the bed is elevated to 30-45 degrees unless contraindicated by the patient’s condition (e.g., certain spinal injuries or surgeries).
- Monitoring Tolerance: Regularly assess the patient’s tolerance to the elevated position and make adjustments as needed to maintain comfort and effectiveness.
Implication:-
- Elevating the head of the bed helps prevent ventilator-associated pneumonia (VAP) and reduces the risk of gastroesophageal reflux and aspiration. Proper positioning enhances respiratory mechanics and supports overall patient comfort and safety.
U: Ulcer Prophylaxis:-
Intervention:-
- Risk Assessment: Assess the patient’s risk for stress ulcers and gastrointestinal bleeding , can use tools like the Glasgow-Blatchford score.
- Prophylactic Treatment: Provide prophylactic treatment with medications such as proton pump inhibitors (PPIs) like Pentoprazole or H2 receptor antagonists like ranitidine.
- Monitoring: Regularly monitor for signs of gastrointestinal bleeding (e.g., hematemesis, melena) and adjust treatment as necessary.
Implication:-
- Preventing stress ulcers and gastrointestinal bleeding is crucial in critically ill patients who are at increased risk due to factors like mechanical ventilation, coagulopathy, and physiological stress. Prophylactic treatment maintains gastrointestinal integrity and prevents complications that could prolong ICU stays and worsen patient outcomes.
G: Glycemic Control:-
Intervention:-
- Blood Glucose Monitoring: Regularly monitor blood glucose levels using bedside glucose meters to maintain target ranges (typically 140-180 mg/dL for critically ill patients).
- Insulin Therapy: Administer insulin therapy as needed to manage hyperglycemia. This may involve continuous insulin infusions or scheduled subcutaneous injections.
- Adjustments Based on Trends: Adjust treatment plans based on blood glucose trends and patient response to ensure effective glycemic control.
Implication:-
- Maintaining appropriate blood sugar levels is essential to prevent both hyperglycemia and hypoglycemia, which can lead to complications such as infections, delayed wound healing, and organ dysfunction. Effective glycemic control supports overall metabolic stability and promotes better recovery outcomes.
S: Spontaneous Breathing Trial:-
Intervention:-
- Daily Assessment: Conduct daily spontaneous breathing trials to evaluate the patient’s ability to breathe without mechanical assistance.
- Criteria for Weaning: Use specific criteria (e.g., stable hemodynamics, adequate oxygenation, appropriate respiratory rate) to determine readiness for weaning and extubation.
- Support During Trials: Provide necessary support during trials, such as adjusting ventilator settings or providing supplemental oxygen as needed.
Implication:-
- Assessing the ability to breathe spontaneously is critical for weaning patients off mechanical ventilation. Successful spontaneous breathing trials indicate readiness for extubation, reducing the risk of ventilator-associated complications and promoting respiratory independence and overall recovery.
B: Bowel Regimen:-
Intervention:-
- Regular Assessment: Regularly assess bowel function and implement a bowel regimen to ensure regular bowel movements. This may include dietary adjustments, stool softeners, laxatives, or enemas.
- Monitoring and Adjustments: Monitor the patient’s response to the bowel regimen and make necessary adjustments to prevent constipation or diarrhea.
Implication:-
- Ensuring regular bowel movements prevents complications such as discomfort, ileus, or bowel obstruction. Effective bowel management supports overall patient comfort, gastrointestinal health, and reduces the risk of further complications.
I: Indwelling Catheter Removal:-
Intervention:-
- Daily Evaluation: Evaluate the necessity of indwelling catheters daily and remove them as soon as they are no longer needed.
- Alternative Methods: Use alternative methods for urine output measurement and management when possible to reduce the need for indwelling catheters.
Implication:-
- Removing unnecessary indwelling catheters reduces the risk of infections such as catheter-associated urinary tract infections (CAUTIs). Timely removal ensures patient safety, reduces healthcare-associated complications, and promotes faster recovery.
D: De-escalation of Antibiotics:-
Intervention:-
- Daily Review: Review antibiotic therapy daily based on clinical progress and culture results to determine the necessity and appropriateness of ongoing treatment.
- Adjustments Based on Data: Adjust antibiotic therapy to narrow the spectrum or discontinue antibiotics when appropriate, based on microbiological data and clinical indications.
Implication:-
- De-escalating antibiotics minimizes the risk of antibiotic resistance and other complications associated with prolonged use of broad-spectrum antibiotics. Targeted treatment ensures effective infection control, reduces unnecessary medication exposure, and supports overall patient safety and recovery.
Conclusion:-
The FAST HUGS BID checklist is an invaluable tool in the critical care setting, ensuring that all aspects of a patient’s needs are addressed comprehensively. By following this mnemonic, healthcare providers can enhance patient outcomes and promote a faster, safer recovery process. Each component of FAST HUGS BID represents a critical aspect of patient care that, when managed effectively, can significantly improve patient outcomes.
Implementing this checklist requires a multidisciplinary approach involving physicians, nurses, pharmacists, dietitians, and other healthcare professionals. By working together, the healthcare team can ensure that each patient receives the highest standard of care, tailored to their specific needs. Regular training and reinforcement of the FAST HUGS BID components can help embed these practices into the daily routine, making comprehensive patient care second nature in the critical care environment.
In summary, the FAST HUGS BID mnemonic is more than just a checklist; it is a framework for delivering holistic, patient-centered care in the intensive care unit. By adhering to these principles ofFAST HUGS BID, healthcare providers can not only address the immediate needs of critically ill patients but also set the stage for long-term recovery and health.
