Table of Contents
ToggleIntroduction:-
Ventilator alarms are crucial for patient safety, signaling potential issues with ventilation that require immediate attention.
This detailed article covers the types of ventilator alarms, their significance, meanings, and how to handle them effectively.
Part 1: Types of Ventilator Alarms
1. High-Pressure Alarms
Significance:-
High-pressure alarms indicate that the pressure required to deliver the set tidal volume is exceeding the set limit. This can be caused by several issues, such as airway obstruction or reduced lung compliance.
Common Causes:-
-
Airway Obstruction :- Mucus plugs, secretions, or kinks in the endotracheal tube.
-
Patient Coughing or Biting the Tube :- Increases airway resistance.
-
Bronchospasm :- Constriction of the airways.
-
Decreased Lung Compliance :- Conditions such as pulmonary edema, ARDS, or pneumothorax.
Management:-
-
Assess and Clear Airway Obstruction :- Suction the patient if needed and check for kinks or blockages in the tubing.
-
Sedation or Reassurance :- If the patient is coughing or biting the tube, provide sedation or reassurance.
-
Administer Bronchodilators :- If bronchospasm is suspected.
-
Evaluate Lung Compliance :- Consider conditions affecting lung compliance and adjust ventilator settings or treat the underlying condition accordingly.
2. Low-Pressure Alarms
Significance:-
Low-pressure alarms indicate that the pressure in the ventilator circuit is lower than the set limit. This can suggest a disconnection or leak in the system.
Common Causes:-
-
Circuit Disconnection :- Tubing disconnected from the ventilator or the patient.
-
Cuff Leak :- The endotracheal tube cuff may be deflated or leaking.
-
Patient Extubation :- The patient may have accidently removed the tube.
-
Loose Connections :- Any loose connections in the ventilator circuit.
Management:-
-
Reconnect the Circuit :- Check and reconnect any disconnected tubing.
-
Check the Cuff :- Inflate the endotracheal tube cuff if it is leaking.
-
Assess for Extubation :- If the patient has removed the tube, prepare for reintubation if necessary.
-
Secure Connections :- Ensure all connections in the ventilator circuit are tight and secure.
3. Apnea Alarm
Significance:-
The apnea alarm sounds when the ventilator does not detect spontaneous breaths within a set period. This is critical in modes where the patient is expected to initiate breaths.
Common Causes:-
-
Central Apnea :- Neurological conditions or medication effects causing the patient to stop breathing.
-
Disconnection or Extubation :- The patient may be disconnected or extubated.
-
Sedation or Over-Medication :- Excessive sedation leading to respiratory depression.
Management:-
-
Assess the Patient :- Check for signs of respiratory effort or consciousness.
-
Reconnect or Reintubate :- Ensure the patient is properly connected to the ventilator and reintubate if necessary.
-
Adjust Sedation :- Modify sedation levels if over-medication is suspected.
-
Activate Backup Mode :- Ensure the ventilator is set to provide mandatory breaths if spontaneous breathing ceases.
4. Low Tidal Volume (Low Vt) Alarm
Significance:-
This alarm indicates that the delivered tidal volume is lower than the set limit, which can impact adequate ventilation and gas exchange.
Common Causes:-
-
Circuit Leak :- Air leak in the ventilator circuit or around the endotracheal tube cuff.
-
Patient-Ventilator Asynchrony :- The patient’s efforts are not synchronized with the ventilator.
-
Partial Obstruction :- Secretions or partial blockage in the airway.
-
Decreased Lung Compliance :- Conditions reducing lung compliance.
Management:-
-
Check for Leaks :- Inspect the ventilator circuit and endotracheal tube cuff for leaks.
-
Synchronize Ventilation :- Adjust ventilator settings to improve synchrony with the patient’s efforts.
-
Clear Obstruction :- Suction the airway to remove any secretions or blockages.
-
Evaluate Lung Compliance :- Assess and treat any underlying conditions affecting lung compliance.
5. High Tidal Volume (High Vt) Alarm
Significance:-
The high tidal volume alarm indicates that the delivered tidal volume exceeds the set limit, which can lead to lung overdistension and potential injury.
Common Causes:-
-
Increased Patient Effort :- The patient is taking larger breaths than the set tidal volume.
-
Ventilator Settings :- Incorrect ventilator settings leading to excessive tidal volumes.
-
Circuit Malfunction :- Issues with the ventilator circuit or settings.
Management:-
-
Evaluate Patient Effort :- Assess the patient’s respiratory effort and adjust ventilator settings if needed.
-
Correct Settings :- Ensure the ventilator settings are appropriate for the patient’s condition.
-
Check for Malfunctions :- Inspect the ventilator and circuit for any malfunctions.
6. High Respiratory Rate (High RR) Alarm
Significance:-
This alarm signals that the patient’s respiratory rate exceeds the set limit, which may indicate distress or inadequate ventilation.
Common Causes:-
-
Patient Anxiety or Pain :- Increased respiratory rate due to anxiety, pain, or discomfort.
-
Hypoxia or Hypercapnia :- Inadequate oxygenation or ventilation.
-
Ventilator Asynchrony :- Poor coordination between the patient’s efforts and the ventilator.
Management:-
-
Assess for Anxiety or Pain :- Provide sedation or analgesia as needed.
-
Optimize Ventilation :- Adjust ventilator settings to improve oxygenation and ventilation.
-
Improve Synchrony :- Adjust the ventilator settings to better synchronize with the patient’s breathing efforts.
Part 2: Detailed Alarm Meanings and Responses
1. High Peak Inspiratory Pressure (PIP) Alarm
Meaning:-
Indicates that the peak pressure in the airways is too high during inspiration.
Detailed Responses:-
-
Check for Obstruction :- Assess for any obstructions in the airway or ventilator circuit. Clear secretions by suctioning the patient.
-
Patient Interaction :- If the patient is coughing or biting the tube, consider providing sedation or repositioning the tube.
-
Bronchospasm Management :- Administer bronchodilators if a bronchospasm is suspected.
-
Assess Lung Compliance :- If decreased compliance is suspected, treat underlying conditions such as pulmonary edema or ARDS.
2. Low PEEP/CPAP Alarm
Meaning:-
Indicates that the set PEEP or CPAP level is not being maintained.
Detailed Responses:-
-
Check for Leaks :- Inspect the ventilator circuit and endotracheal tube cuff for air leaks.
-
Ensure Proper Setup :- Verify that the PEEP/CPAP settings are correctly configured and the patient is properly connected.
-
Evaluate Patient Condition :- Ensure the patient is not exhaling forcefully or disconnecting from the ventilator.
3. Disconnection or Circuit Disconnect Alarm
Meaning:-
Indicates that the ventilator circuit has become disconnected from the patient or the ventilator.
Detailed Responses:-
-
Immediate Reconnection :- Reconnect the ventilator circuit to the patient and check all connections.
-
Secure All Connections :- Ensure all tubing and connections are tight and secure.
-
Monitor Patient :- Continuously monitor the patient for signs of respiratory distress and take immediate action if necessary.
4. High Minute Ventilation (High Ve) Alarm
Meaning:-
Indicates that the total volume of air delivered per minute is higher than the set limit.
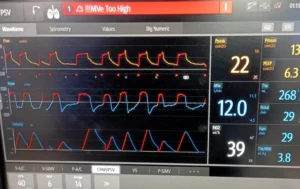
Detailed Responses:-
-
Assess Patient Effort :- Determine if the patient is breathing rapidly or taking deep breaths.
-
Review Ventilator Settings :- Ensure that the settings are appropriate for the patient’s condition.
-
Check for Hyperventilation :- Assess for underlying causes of hyperventilation, such as anxiety, pain, or metabolic acidosis, and address them accordingly.
5. Low Minute Ventilation (Low Ve) Alarm
Meaning:-
Indicates that the total volume of air delivered per minute is lower than the set limit.
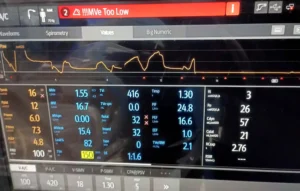
Detailed Responses:-
-
Evaluate for Leaks :- Inspect the ventilator circuit and endotracheal tube for leaks.
-
Assess Patient’s Breathing Effort :- Determine if the patient’s breathing effort is inadequate and provide necessary support.
-
Check Ventilator Settings :- Ensure the settings are appropriate and the ventilator is delivering the set volumes.
6. High FiO2 Alarm
Meaning:-
Indicates that the fraction of inspired oxygen (FiO2) being delivered is higher than the set limit.
Detailed Responses:-
-
Review Settings :- Check the ventilator settings to ensure the FiO2 is set correctly.
-
Assess Oxygen Source :- Verify that the oxygen source is functioning properly and not delivering excessive oxygen.
-
Evaluate Patient’s Oxygen Needs :- Determine if the patient requires a higher FiO2 and adjust settings accordingly if clinically indicated.
Part 3: Handling Specific Alarms and Scenarios
Scenario 1: Handling a High-Pressure Alarm
-
Immediate Actions:-
-
Check for kinks or obstructions in the ventilator circuit.
-
Suction the patient to clear any secretions.
-
Assess the patient for coughing or biting the tube and provide sedation if needed.
-
-
Further Assessment:-
-
Evaluate for conditions that reduce lung compliance, such as pulmonary edema or ARDS.
-
Consider a bronchodilator if bronchospasm is suspected
-
-
Documentation:-
-
Document the alarm, the cause identified, and the actions taken.
-
Record any changes in ventilator settings or medications administered.
-
Scenario 2: Handling a Low-Pressure Alarm
-
Immediate Actions:-
-
Check for disconnections in the ventilator circuit and reconnect if needed.
-
Inflate the endotracheal tube cuff if it is leaking.
-
-
Further Assessment:-
-
Ensure the patient has not self-extubated.
-
Verify that all connections are secure and properly fitted.
-
-
Documentation:-
-
Document the alarm, the cause identified, and the actions taken.
-
Record any patient assessments and interventions.
-
Scenario 3: Handling an Apnea Alarm
-
Immediate Actions:-
-
Assess the patient’s consciousness and respiratory effort.
-
Reconnect the ventilator circuit if disconnected and prepare for reintubation if needed.
-
-
Further Assessment:-
-
Adjust sedation levels if over-sedation is suspected.
-
Ensure backup ventilation modes are activated.
-
-
Documentation:-
-
Document the alarm, the cause identified, and the actions taken.
-
Record any changes in patient status or ventilator settings.
-
Scenario 4: Handling a Low Tidal Volume Alarm
-
Immediate Actions:-
-
Check for leaks in the ventilator circuit and endotracheal tube cuff.
-
Suction the patient to clear any obstructions.
-
-
Further Assessment:-
-
Assess and improve patient-ventilator synchrony.
-
Evaluate and treat conditions affecting lung compliance.
-
-
Documentation:-
-
Document the alarm, the cause identified, and the actions taken.
-
Record any adjustments to ventilator settings or patient interventions.
-
Scenario 5: Handling a High Respiratory Rate Alarm
-
Immediate Actions:-
-
Assess the patient for anxiety or pain and provide sedation or analgesia as needed.
-
Increase oxygen delivery if hypoxia is suspected.
-
-
Further Assessment:-
-
Ensure the ventilator settings are appropriate for the patient’s condition.
-
Improve synchrony between the patient and the ventilator.
-
-
Documentation:-
-
Document the alarm, the cause identified, and the actions taken.
-
Record any changes in patient status or ventilator settings.
-
